A Patient’s Guide to Anatomic Total Shoulder Replacement (Standard Shoulder Shoulder)
Introduction
Yearly, there are approximately 50,000 shoulder replacements performed annually in the USA. Anatomic shoulder replacements were introduced in 1970 by Dr. Charles Neer. The early designs for shoulder replacement and subsequent design improvements have vastly increased the number of procedures performed per year. Anatomic shoulder replacement is indicated for patients with refractory pain in the shoulder due to osteoarthritis. An anatomic replacement requires an intact rotator cuff to function effectively. Dr. Groh is the chief designer of the shoulder replacement you will receive for this condition.
Anatomy
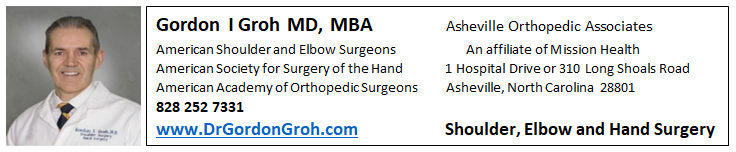
The shoulder serves as a connection between the chest and arm. The clavicle functions as a strut connected to the shoulder bone (scapula). The scapula articulates with the humerus and accounts for approximately 70% of shoulder motion (the remaining motion occurs between the scapula and the thorax). Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
A right shoulder viewed from the front showing the clavicle, humerus and scapula.
The motion between the shoulder blade and scapula is a stable gliding surface over bursal structures and not prone to dislocation. However, the articulation between the humerus and scapula has little bony stability. This is because the ball of the humerus is large and the socket is small on the scapular side—think of the small amount of stability a golf ball has on a tee.
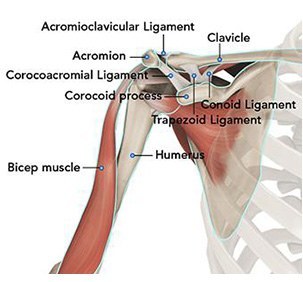
The inside layer of muscles gives the shoulder stability and motion above shoulder height and is called the rotator cuff—a series of 4 muscles
The muscles underlying the deltoid—the rotator cuff viewed from the back and front
Because of the necessity for the rotator cuff to stabilize the ball of the humerus, an anatomic or standard shoulder replacement is indicated when arthritis of the shoulder is coupled with an intact rotator cuff. This combination is the most common in patients with osteoarthritis
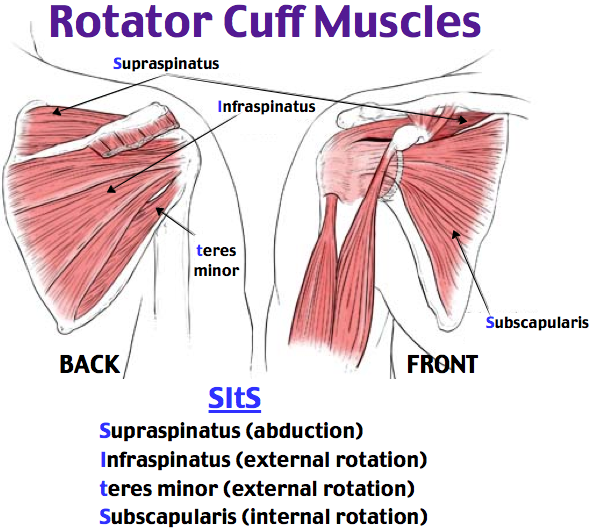
A diagram of an anatomic shoulder replacement—the plastic socket replaces the cup of the scapula (shoulder blade). A metal ball component replaces the worn humeral head.
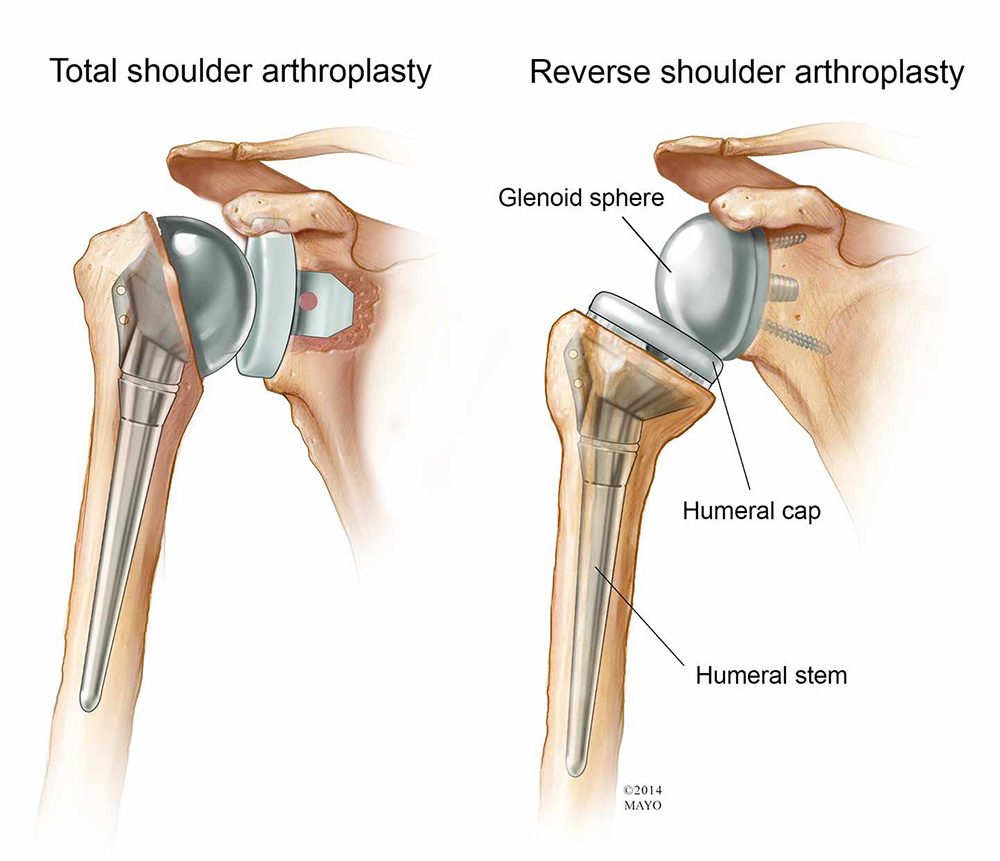
On the left is a standard (anatomic) shoulder arthroplasty. The components of the ball and cup are reversed on the right—a reverse shoulder replacement.
Diagnosis
Symptoms
Patients report pain and limitation in raising the arm with shoulder osteoarthritis. This greatly limits the function of these patients—many are unable to get a glass from a shelf, comb their hair or reach across the table to grab the salt shaker. Pain may be worse at night and interfere with sleeping.
Surgeon Examination
After reviewing the patient’s symptoms, a review of their pertinent medical history and family history is obtained. The range of motion of the shoulder is measured in multiple planes. The strength of the shoulder in resisting motions is tested.
Imaging
X-rays can determine the amount of arthritis associated with the disease. Typically x-rays from multiple angles better discern the amount of arthritis. Patients with chronic rotator cuff tearing may exhibit changes in relationship of the ball and socket which indicates a massive chronic tear with a high riding humeral head. Patients with an intact rotator cuff typically have a head centered on the glenoid.
Enhanced imaging of CT or MRI may be used to further image bone for reconstruction. MRI may be used to evaluate the status of the rotator cuff when it is unclear regarding the rotator cuff integrity. In intact rotator cuff is typically required for anatomic shoulder replacement.
Treatment
Nonoperative
Initial management for shoulder arthritis mirrors osteoarthritis in other joints. First line treatment includes the utilization of anti-inflammatory medications (Advil, Aleve). Tylenol may help patient with pain and may be utilized concurrently. For many patients, heat is a useful adjuvant to improve pain.
For patients with continued pain, a steroid injection of the shoulder joint may be indicated. These injections may be done in connection with mediations listed above. The role of physical therapy for shoulder arthritis remains unclear. Typically, shoulder steroid injections may be repeated 2-3 times per year. Risks with injection include depigmentation, tendon rupture, and infection.
Operative
For patients with continued pain and poor function, shoulder arthroplasty is an excellent option. Results are shown in all studies to correlate with surgeons who do a considerable volume of shoulder replacement every year. The average orthopedic surgeon performs less than five shoulder replacements per year. Dr. Groh performs over 175 shoulder replacements in an average year.
The anesthesia choices include regional or general anesthesia. Incisions are required to place hardware for the reverse procedure into position. Dissection to identify nerves and bone landmarks usually makes for an exacting procedure—requiring a subspecialist.
Dr. Groh performs over 90% of shoulder replacement surgery as an outpatient. Surgery is typically performed with a nerve block and supplemental anesthesia. Surgery typically requires less than 90 minutes, and the risks of blood transfusion are 1% in most studies.
The length of incision for a typical shoulder replacement is two inches in females and three inches in muscular males. Dr. Groh utilizes negative pressure wound management systems to improve wound healing and decrease the risk of infection. Patients may shower as desired with this wound management system and do not need to change dressings at home.

Postoperative incision prior to closure for shoulder replacement in a muscular male—measuring seven centimeters (just under three inches)


Negative pressure wound management system in place at the conclusion of shoulder replacement. The surgical incision is approximately half the size of the purple wound management sponge.
The need for medical prevention of deep vein clots after surgery is controversial and ranges from none to aspirin, to mechanical compression, to blood thinning agents. Other standard risks associated with surgery and arthroplasty are applicable to these types of procedures.
WATCH AN ANIMATION VIDEO OF STANDARD (ANATOMIC) SHOULDER REPLACEMENT
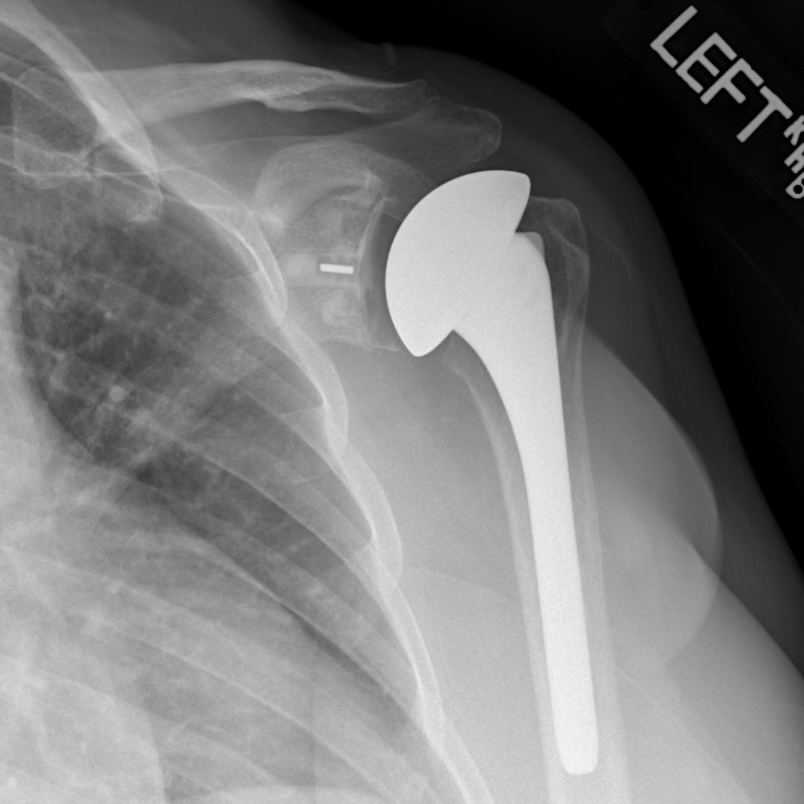
A postoperative x-ray of left total shoulder viewed from the front
Rehabilitation
After surgery the arm is immobilized in a sling to allow for wound healing. Patients report pain after surgery, but the pain generally improves after the first day and utilization of multimodal pain techniques have been shown to improve outcomes for patients. Most patients will report resolution of their preoperative deep achy pain within the first two weeks and note their pain from the surgery has subsided considerably.
Many studies have shown that patients can successfully rehabilitate their shoulder on their own at home. Patients are typically guided through a therapy program and weaned from their sling over the first 2 months. Ingrowth of the components typically requires 3-4 months and patients may return to golf by 4 months after surgery. Continued work on motion and strength allows form improvement for up to 1 year after surgery.
Dr. Groh is an expert shoulder replacement surgeon
- Named top 60 Shoulder Surgeon in the USA by Becker’s Orthopedics
- Chief Designer for Shoulder Replacement Implants—Both Anatomic and Reverse Shoulders—Marketed Worldwide by DJO/Encore Orthopedics
- Active member of the American Shoulder and Elbow Surgeons
- Written 50 Articles and Textbooks on Shoulder Injuries
- Holds multiple shoulder implant device patents