A Patients Guide to Pectoralis Major Rupture or Pectoralis Tear (Pec Tear)
Introduction
The pectoralis muscle is located on the front of your chest. It is attached to the bone of the upper arm/shoulder by tendons—strong cords of fibrous tissue that attach muscle to bones
Tears of the pectoralis tendon are uncommon. They are most often caused by a sudden eccentric force. The injury is almost exclusively in males and most injuries are associated with weightlifting.
Once the pectoralis is torn away from the shoulder bone (humerus), it will not grow back and heal because the muscle tissue retracts the tendon away. Other arm muscle make it possible for the shoulder to move well without the pectoralis muscle. However, they cannot fulfill all the functions of the shoulder, especially the motions of adducting the shoulder (pulling it across the chest) and internally rotating the shoulder with force.
To return arm strength to near normal levels, surgery to repair the torn tendon is usually recommended. However, nonsurgical treatment is a reasonable option for patients who may have only muscular partial tear of the pectoralis and not require full arm function.
Anatomy
The pectoralis muscle includes both a major and a minor component. The pectoralis minor inserts on the coracoid process of the shoulder blade and injury to it is uncommon and typically does not require surgical correction. Indeed, many surgical repairs for instability release this muscle from its insertion deliberately—without any reported deficits
The pectoralis major muscle has both a sternal (breastbone) and clavicular head. The muscle inserts on the humerus just lateral to the bicipital groove. The pectoralis major is a large muscle and contributes significant strength to the upper arm.
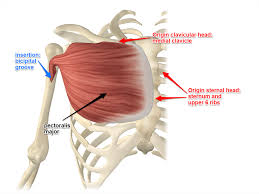
Pectoralis major origins and insertions
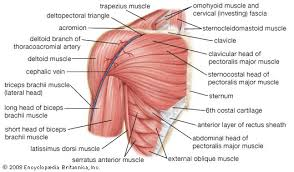
Detailed anatomy of the shoulder
Cause
Rupture of the pectoralis major is uncommon although increasing in incidence. The injury typically occurs in males between ages 20 and 40 years. Most cases occur in weightlifters doing chest exercises. The injury occurs with excessive tension on a maximally contracted muscle and the most commonly occurs with the pectoralis tendon tearing away from the bone (tendinous avulsion).
Classification of Injury
Although tendinous disruption is the most common injury pattern—fewer common degrees and locations have been described. The classification below lists the patterns:
Modified Tietjen (Anatomic) Classification
Type Description
I Muscle contusion or sprain
II Partial tear
III Complete tear (further subclassified by location)
Location
A Muscle origin
B Muscle belly
C Myotendinous junction
D Tendon avulsion off humerus (no bone)
E Bony tendon avulsion off humerus
F Tendinous rupture
Symptoms
Typically, the patient will report a sudden pop or a tearing sensation occurring during a chest exercise. The pop or tearing is typically associated with pain and weakness of the shoulder

An acute right pectoralis tendon rupture during bench press exercise
Doctor Examination
Physical Examination
After discussing your symptoms and how the injury occurred, your doctor will examine your chest and shoulder. During the physical examination, your doctor will feel the front of your chest, looking for a gap in the tendon. Inspection and palpation will typically reveal:
- swelling and bruising of anterolateral chest wall and/or proximal arm
- “dropped nipple” sign – ipsilateral nipple will appear lower than the unaffected side due to medial retraction of muscle belly
- palpable defect and loss of anterior axillary contour – accentuated by resisted adduction

A left pectoralis major tear. Note the loss of muscle in the axillae (armpit), bruising along chest and arm, and the lower nipple on the left side
Imaging Tests
In addition to the examination, your doctor may recommend imaging tests to help confirm a diagnosis.
X-rays. Although x-rays cannot show soft tissues like the pectoralis tendon, they can be useful in ruling out other problems that can cause shoulder pain.
Ultrasound. This imaging technique can show the free end of the pectoralis tendon that has recoiled up in the arm.
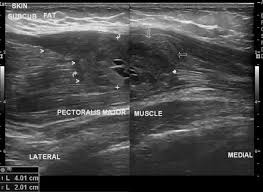
Ultrasound of a pectoralis major rupture
Magnetic resonance imaging (MRI). These scans create better images of soft tissues. They can show both partial and complete tears of the pectoralis tendon. However, there may be enough information from the history and physical examination that an MRI is not need by an experienced physician. Further, MRI scans must be ordered of the specific pectoralis area. A typical “shoulder” MRI will not image the pectoralis and the exam may be read as “normal”, giving a false negative for the test. Proper MRI imaging is essential for pectoralis evaluation.

MRI of left shoulder showing a tear and retraction of the pectoralis major tendon (white arrow).
Treatment
Surgery to reattach the tendon to the bone is necessary to regain full arm strength and function.
Nonsurgical treatment may be considered if you are older and less active, or if the injury occurred in your nondominant arm and you can tolerate not having full arm function. Nonsurgical treatment may also be an option for people who have medical problems that put them at higher risk for complications during surgery.
Nonsurgical Treatment
Nonsurgical treatment options focus on relieving pain and maintaining as much arm function as possible. However, patients treated without surgery will always have a strength deficit and continue cosmetic changes of the pectoralis rupture. Treatment recommendations may include:
- Rest. Avoid heavy lifting and overhead activities to relieve pain and limit swelling. Your doctor may recommend using a sling for a brief time.
- Nonsteroidal anti-inflammatory medications. Drugs like ibuprofen and naproxen reduce pain and swelling.
- Physical therapy. After the pain decreases, your doctor may recommend rehabilitation exercises to strengthen surrounding muscles in order to restore as much movement as possible.
Surgical Treatment
Surgery to repair the tendon should be performed during the first 2 to 3 weeks after injury. After this time, the tendon and biceps muscle begin to scar and shorten and restoring arm function with surgery may not be possible. While other options are available for patients requesting late surgical treatment for this injury, they are more complicated and generally less successful.
Procedure
There are several different procedures to reattach the pectoralis tendon to the shoulder bone. A common surgical option is to attach the tendon with stitches through holes drilled in the humerus bone. Another method is to attach the tendon to the bone using small metal implants (called suture anchors).
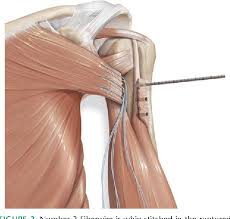
Sutures in the pectoralis tendon tear of a left shoulder viewed from the front.
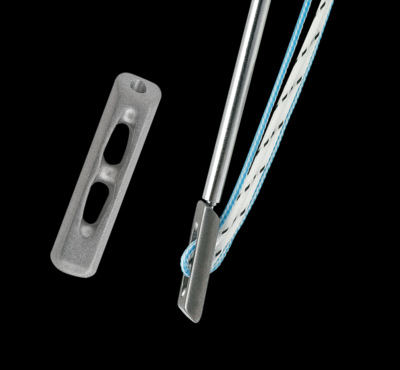
A commonly used suture anchor for pectoralis tendon repairs left (the anchor is approximately 5 mm). The right image showed the anchor with the suture and inserter. The inserter is removed after positioning the anchor.
The procedure may be performed as an outpatient surgery utilizing a combination of regional and or general anesthesia. The procedure typically requires just over an hour of time and blood loss is minimal. An experienced surgeon should be able to accomplish the procedure through a small incision.
Complications of surgery are rare, but may include standard surgical risks including infection and bleeding. The chances of retearing the pectoralis repair are thought to be low, at about 5%.
Rehabilitation
After surgery, the arm is immobilized in a sling to allow for wound healing. Patients report pain after surgery, but the pain generally improves after the second day and utilization of multimodal pain techniques have been shown to improve outcomes for patients. Night pain is typically the most problematic—but multimodal pain programs, heat, and sleeping elevated can improve this difficulty.
Many studies have shown that patients can successfully rehabilitate their shoulder on their own at home. Patients are typically guided through a therapy program and weaned from their sling over the first 8-12 weeks. Ingrowth of the tendon typically requires 4 months and patients may return to golf by 5-6 months after surgery. Continued work on motion and strength allows form improvement for up to 1 year after surgery.
Dr. Groh is an expert shoulder surgeon
- Named top 60 Shoulder Surgeon in the USA by Becker’s Orthopedics
- Active member of the American Shoulder and Elbow Surgeons
- Written 50 Articles and Textbooks on Shoulder Injuries
- Holds patents and developed multiple shoulder implants and devices