A Patient’s Guide to Frozen Shoulder (Adhesive Capsulitis)
Introduction
Adhesive capsulitis or a frozen shoulder is a condition which combines limitation of shoulder motion (frozen) and often pain. The disease appears in most cases to be self-limited, but can take two years to resolve without treatment. Approximately 6% of the USA population will suffer from frozen shoulder at some point in their life.
Frozen shoulder may be associated with trauma from fractures or surgery, but commonly there is no known inciting event—idiopathic cause. The disease is more prevalent in diabetics—approximately 15% of patients with diabetes will experience the disease. Frozen shoulder is more common in women rather than men. Interestingly, once the shoulder recovers from the disease, it will not recur again in the same shoulder. However, the opposite shoulder is at increased risk of experiencing the disease over the course of a lifetime.
While the cause of adhesive capsulitis remains unknown, the course of the disease from onset to resolution follows a fairly regular timeline—freezing, frozen, and thawing. Medical intervention can speed the course of resolution of the disease and improve the pain associated with the condition.
Anatomy
The shoulder serves as a connection between the chest and arm. The clavicle functions as a strut connected to the shoulder bone (scapula). The scapula articulates with the humerus and accounts for approximately 70% of shoulder motion (the remaining motion occurs between the scapula and the thorax). Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
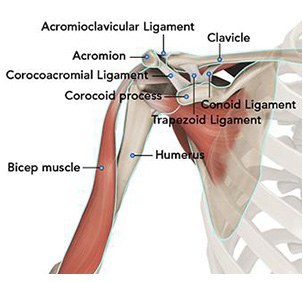
A right shoulder viewed from the front showing the clavicle, humerus and scapula.
The motion between the shoulder blade and scapula is a stable gliding surface over bursal structures and not prone to dislocation. However, the articulation between the humerus and scapula has little bony stability. This is because the ball of the humerus is large and the socket is small on the scapular side—think of the small amount of stability a golf ball has on a tee.
Your shoulder is a ball-and-socket joint made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
The head of the upper arm bone fits into a shallow socket in your shoulder blade. Strong connective tissue, called the shoulder capsule, surrounds the joint. To help your shoulder m0ve more easily, synovial fluid lubricates the shoulder capsule and the joint.
The inside lining of the shoulder is the cartilage which allows for smooth gliding of the ball and socket. The cartilage does not have direct blood supply, rather it obtains nutrients from the tissue lining the joint call the synovium. In frozen shoulder, the lining synovium becomes inflamed and constricted forming adhesions in the joint.
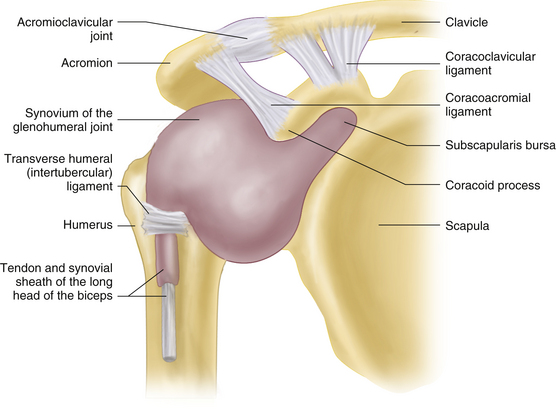
A right shoulder viewed from the front. The synovium (blue arrow) lines the articular surfaces of the humerus (humeral head and glenoid of scapula)
Diagnosis
Symptoms
Patients report uniformly decreased range of motion with the condition. Placing the arm above the shoulder is limited. Patients complain of difficulty with activities of reaching up to a shelf. Similarly, reaching behind the back becomes difficult—threading a belt or grabbing a wallet.
Pain is reported according to the stage of the disease. Initially in the freezing stage the shoulder becomes less mobile, but pain is not a predominant factor. As the shoulder moves into the frozen stage, motion becomes even more restricted and pain may become more prevalent. Finally, as the shoulder begins to thaw—most patients will report more pain as the shoulder motion improves.
Surgeon Exam
After noting your symptoms and associated history (trauma, diabetes) a physical examination is undertaken. The range of motion of the joint is measured. The ability of the arm to externally rotate is correlated with its ability to elevate overhead (Codman’s paradox). The neurovascular status is checked for the arm and range of motion of the neck looks to reveal any cervical spine nerve issues which may affect the patient.
Imaging Studies
Routine x-rays for frozen shoulder do not typically yield additional information, but may exclude other diagnosis including osteoarthritis, rheumatoid arthritis, and trauma—all of which may present with pain and stiffness.
Advanced imaging CT and MRI is typically not required to make the diagnosis of a frozen shoulder. These studies may add additional information regarding soft tissue and bone around the shoulder, but are not necessary for the diagnosis.
Treatment
It is important to remember the time course for improvement in frozen shoulder. Quick recovery from the disease is not a hallmark of the process.
Initial steps are correlated with the disease stage and centered on return of motion and improvement in pain. Improvements in motion are gained by a stretching program. The program may be completed at home or under the direction of a physical therapist. Both mechanisms have been shown to be effective, although some studies have shown greater improvement with home shoulder stretching alone.
Pain associated with the disease is correlated with the stage. Pain may be treated with anti-inflammatory oral medications (Motrin, Aleve), Tylenol, or in some cases mild medications in the narcotic family (Ultram, Norco). Night pain is typically reported as the worst time for most patients and interference with sleep is common. However, the use of sleeping medications is not generally recommended for this condition.
Heat is a useful adjuvant for treating a frozen shoulder. Often the application of heat prior to sleeping improves night time dysfunction. Similarly, heat during the day may improve symptoms as well. Application of heat prior to stretching often improves the amount of stretch patient’s report they can achieve.
In addition to stretching, studies have shown that injection of steroid into the joint can often make the recovery from frozen shoulder more rapid. These injections are typically performed in the surgeon’s office with local anesthetic. Some patients may experience immediate improvement in motion and pain, but the majority will need to continue with their regular program and expect improvement over time.
Other treatments are described including a manipulation of the shoulder under regional or general anesthesia to break the adhesions. This procedure may be done in conjunction with an arthroscopy to release adhesions. However, most patients do not require these procedures a serious complications including fracture, rotator cuff tear, and nerve injury have been reported.