A Patient’s Guide to Dupuytren’s Disease
Introduction
Dupuytren’s disease is a condition that affects fingers and thumbs in the hand. The condition slowly evolves over time and develops cords and nodules which may limit the ability of the fingers or thumb to straighten. The inability to straighten digits can adversely effect hand function. Patients with Dupuytren’s may report difficulty with putting on gloves or reaching into a pocket. Similarly gripping larger objects may become difficult as the disease progresses and the contractures become more severe.

Picture of patient with severe Dupuytren’s of the ring finger—note the inability to straighten the digit due to the cord (arrow).
Anatomy
The palm of the hand and fingers are covered by a connective tissue called fascia. This fascia is composed of collagen. This fascia plays a key role in the stability of our palmar skin in the ability to manipulate, grasp, and hold objects.
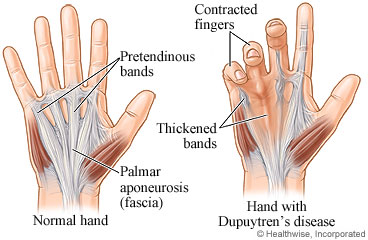
In a normal hand the palmar fascia forms the palmar aponeurosis and the paratendinous bands.
In Dupuytren’s disease, this normal fascia undergoes adverse changes. The collagen becomes more cord like and may form nodules. Beside the changes in the fascia, smooth muscle cells also proliferate. The combination of these two processes cause the digit to be unable to extend. The disease is progressive and more severe involvement tends to occur over time.
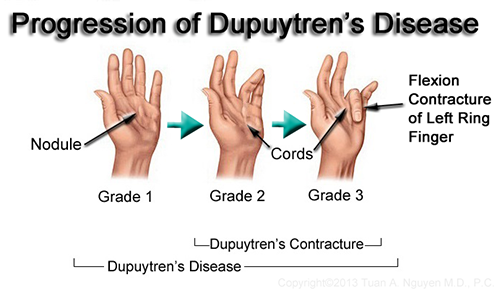
Dupuytren’s disease progression in the left hand ring finger over time
Although the exact cause of Dupuytren’s is unknown, certain associations are understood. The disease is more prevalent in patients whose ancestors originate from Northern Europe. The disease has a strong family history component. Men tend to be far more affected than women. Most patients are over age 50 at the onset of disease. Other factors such as alcohol use and hand exposure are not thought currently to play a significant role.
Diagnosis
Symptoms
Most patients present with an inability to extend the digit. Some patients may complain of pain and based on the severity of the contracture—difficulty with function. Patients who develop the disease in the 7th decade of life or older are less likely to have significant progression. Similarly, patients whose families have a strong disposition toward the disease typically have more aggressive progression.
Hand Surgery Examination
After noting the patient’s symptoms, the hand surgeon notes the involvement of the hand. The locations of pits, nodules and cords are recorded—along with their severity. The range of motion of the digits is recorded—as well as the ability to place the hand palm down in a flat position.
Imaging Studies
X-rays or other advanced imaging studies are typically not required for Dupuytren’s diagnosis or treatment
Treatment
Nonoperative
If the patients Dupuytren’s is mild and not affecting function, observation may be indicated. These patients typically are able to place the palm flat and do not have involvement of the smaller finger joints (interphalangeal joints). Observation over time may be indicated as the disease may progress to interfere with function
Operative
Injection of Collagenase
Since the cords of Dupuytren’s are composed of collagen, enzymatic treatment with collagenase can rupture the cord—allowing the digit to straighten. This procedure is typically done in the office and a manipulation may be necessary in 24-48 hours. Local anesthesia may be utilized in the treatment.
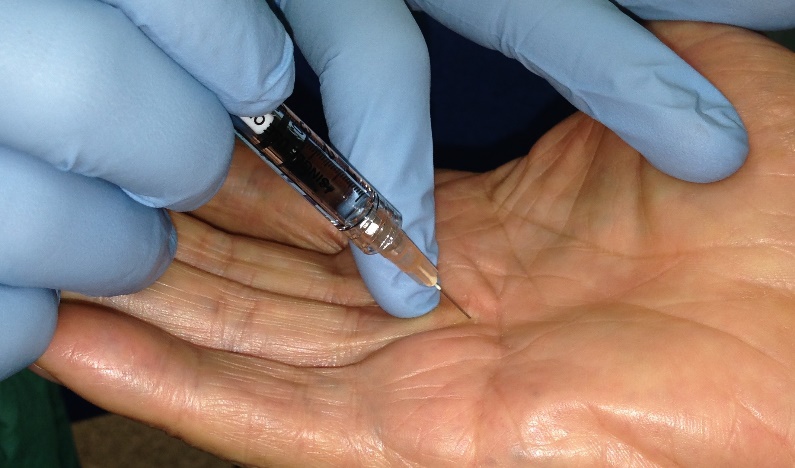
Injection of a Dupuytren’s cord.
Injection of collagenase may require multiple injections. The cord is initially ruptured, but recurrence of the disease is difficult to predict, but early recurrence may occur.
The same goals are attempted with needle aponeurotomy. This procedure may be performed in an office or operating room and aims to disrupt cords utilizing a needle without collagenase. The risks of both treatments include infection, tendon rupture or nerve injury
Operative Treatment
For patients whose disease progresses to interfere with function, operative management may be considered. This procedure can be performed as an outpatient surgery under regional anesthesia. In open surgery, the goal is to identify normal tissue and resect diseased tissue—a palmar and digital fasciectomy.
Resection of the diseased tissue commonly allows for the digit to straighten. Uncommonly skin deficits may arise requiring local wound care or skin grafting. Initially, the skin incisions for the procedure are prevalent, but fade over time.


Left image–Initial incisions which are shaped like a Z to allow normal skin to be brought into position with the fasciectomy. Right image—early healing after suture removal
Postoperatively, patients are discharged to home and should follow instructions regarding elevation, activity, and use of pain medication. After surgery, patients are typically immobilized in a splint for one week and return to the office for a wound check.
Rehabilitation
Most patients will be instructed to see a hand therapist to begin range of motion and fitting for bracing. Sutures are typically removed around 2 weeks after surgery. Stiffness and swelling are expected after surgery and regress over time. Because of the extensive dissection, some patients will have some finger numbness after surgery which improves. Work with the hand therapist maximizes function and cosmetic after surgery.
Outcomes
Although there is good treatment for Dupuytren’s, there is no cure. Recurrences may occur regardless of the technique chosen for treatment. Complications with surgery are rare, but may occur—significant disease progression or joint disease may limit the ability to gain motion after surgery.