A Patient’s Guide to Radial Head Fractures of the Elbow
Introduction
Fractures of the radial head are common elbow fractures Most fractures are associated with trauma—and many are associated with trauma. Radial head fractures may occur in isolation or associated with other fractures of the elbow.
Most radial head fractures occur in adults and are more common in men rather than women.
Anatomy
The elbow serves two distinct functions: 1) to bend and straighten 2) to turn the palm up and palm down. The elbow utilizes three bones in articulation to accomplish these purposes—humerus, ulna, and radius.
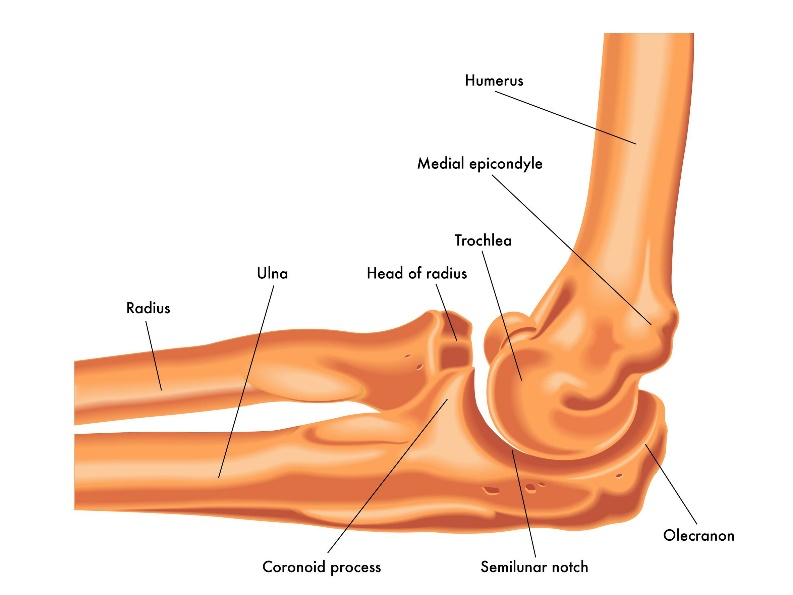
Lateral view of a right elbow demonstrating humerus, ulna, and radius. The radial head is identified with the arrow
The bones of the elbow are held together by joint capsule, ligaments and tendons. As we age, the strength of both ligaments and bones decrease over time.
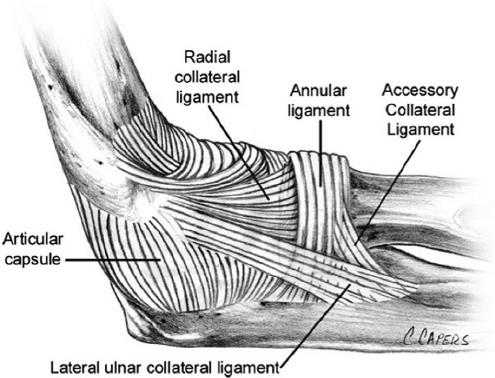
Ligaments of the elbow viewed from the lateral aspect
Diagnosis
Symptoms
Patients who experience distal humerus fractures present with pain, swelling and often bruising over time. There may be deformity of the arm dependent upon the degree of displacement of the fracture.
Physician Exam
After taking a history and noting your symptoms, a physical exam is then performed by the surgeon. The status of the vascular supply to the hand is observed. Similarly the sensation and motion of digits are noted. Although uncommon, fractures in this area may embarrass vascular supply secondary to injury or swelling. Similarly, nerve function may be disrupted due to trauma or displacement of fractures.
Imaging
X-rays are indicated to determine the bones which have been injured and if there are any dislocations associated with the injury. X-rays may be taken from several angles to better delineate the fracture.

A lateral view of a left elbow showing a displaced radial head fracture. The displaced fragment is denoted with an arrow
In many cases, x-rays alone may adequately provide enough information to determine treatment. However, additional imaging for bone, such as computerized tomography (CT scan) may yield additional helpful information. If more concern is directed toward ligament or tendon injury, MRI imaging may be ordered.
Treatment
Nonoperative
Nonoperative treatment is reserved for nondisplaced and minimally displaced fractures currently. In the past, extensively comminuted fractures were not amenable to surgical management and therefore treated without surgery—this is rarely the case today. Nonoperative management usually requires some period of immobilization, followed by supervised range of motion. Stiffness is problematic with elbow fractures in general and may be more pronounced with longer immobilization. Difficulties with gaining palm up and extension of the elbow are the most problematic motion arcs to regain.
Operative
Displaced fractures typically require operative management. The goals of operative treatment is to alignment the fracture and the cartilage surfaces. The cartilage surfaces are the gliding mechanism by which the elbow moves. Typically, better alignment is associated with better function. Fractures with less than three larger fragments may be candidates for open reduction and internal fixation with screws or plates. Fractures which show extensive comminution may be candidates for replacement of the radial head.
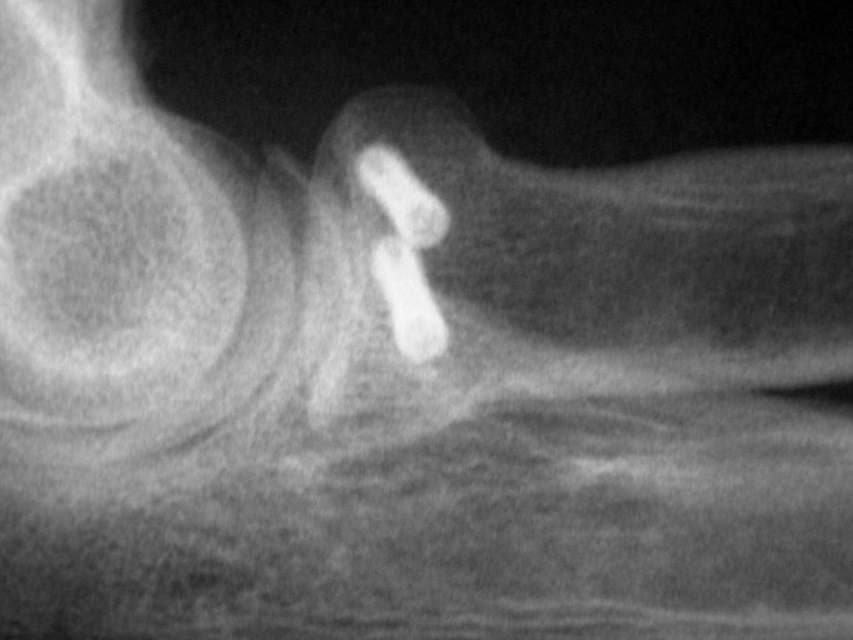
A lateral view x-ray of a radial head fracture treated with screws
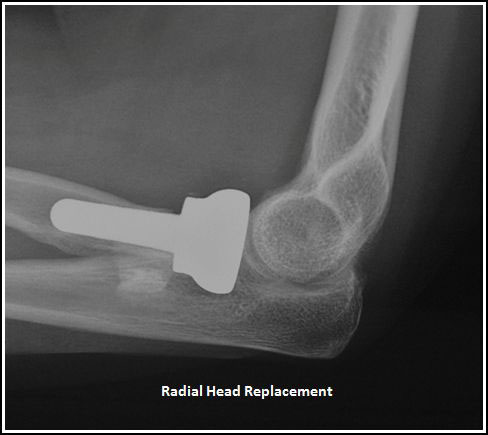
A lateral x-ray of a radial head fracture treated with a radial head replacement
These fractures are typically complex and require specialized care. The anesthesia choices include regional or general anesthesia. Isolated fractures may be treated on an outpatient basis.
Rehabilitation
After surgery the arm is immobilized in a splint to allow for wound healing. The ability to gain stable fixation determines the amount of motion allowed for the elbow, as well as the postoperative timing. Bracing may be used in the postoperative period to control motion and formal therapy is often a useful adjuvant for care. Patients report pain after surgery, but the pain generally improves as the fracture fragments are stabilized. Initiation of therapy causes soreness for many patients.
Fracture healing requires 8-12 weeks and many patients require months of therapy to reach maximum improvement. Improvement over the injury state occurs for most individuals resulting in a functional elbow. However, even under the best of circumstances–some limitation of motion, soreness, and stiffness may result. Arthritis associated with posttraumatic arthritis may result from these severe injuries. Other complications can include infection, nerve injury, nonunion of bones, and painful hardware.