A Patient’s Guide to Mallet Finger (Baseball Finger)
Introduction
Mallet finger is an injury to the thin tendon that straightens the end joint of a finger or thumb. Although it is also known as “baseball finger,” this injury can happen to anyone when an unyielding object (like a ball) strikes the tip of a finger or thumb and forces it to bend further than it is intended to go. As a result, you are not able to straighten the tip of your finger or thumb on your own.

With a mallet finger injury, the fingertip droops and cannot be actively straightened.
Anatomy
Tendons are tissues that connect muscles to bone. The muscles that move the fingers and thumb are in the forearm. Long tendons extend from these muscles through the wrist and attach to the small bones of the fingers and thumb.
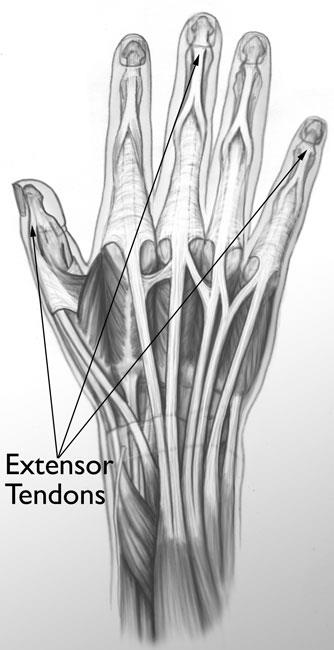
The extensor tendons on the top of the hand straighten the fingers. The flexor tendons on the palm side of the hand bend the fingers.
The extensor tendons straighten the fingers and thumb through a very complex arrangement.
Description
In a mallet injury, when an object hits the tip of the finger or thumb, the force of the blow tears the extensor tendon. Occasionally, a minor force such as tucking in a bed sheet will cause a mallet finger.
The injury may rupture the tendon or pull the tendon away from the place where it attaches to the finger bone (distal phalanx). In some cases, a small piece of bone is pulled away along with the tendon. This is called an avulsion injury.
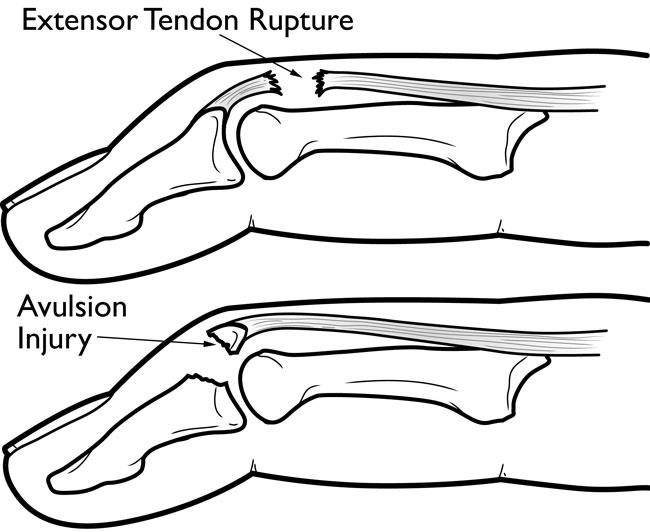
(Top) A rupture of the extensor tendon.
(Bottom) A fragment of the distal phalanx has pulled away with the tendon.
The long, ring, and small fingers of the dominant hand are most likely to be injured.
Symptoms
The finger is usually painful, swollen, and bruised. The fingertip will droop noticeably and will straighten only if you push it up with your other hand.
Doctor Examination
A mallet finger injury requires medical treatment to ensure the finger regains as much function as possible. Most doctors recommend seeking treatment within a week of injury. However, there have been cases in which treatment was delayed for as long as a month after injury and full healing was still achieved.
Physical Examination
After discussing your medical history and symptoms, your doctor will examine your finger or thumb. During the examination, your doctor will hold the affected finger and ask you to straighten it on your own. This is called the mallet finger test.

During a mallet finger test, your doctor determines whether you can straighten your fingertip without assistance.
X-Rays
Your doctor will most likely order x-rays of the injury. If a fragment of the distal phalanx was pulled away when the tendon ruptured, or if there is a larger fracture of the bone, it will appear in an x-ray. An x-ray will also show whether the injury pulled the bones of the joint out of alignment.

X-ray shows that a piece of the distal phalanx bone broke away with the tendon.
Treatment
Mallet finger injuries that are not treated typically result in stiffness and deformity of the injured fingertip. Most mallet finger injuries can be treated without surgery.
In children, mallet finger injuries may involve the cartilage that controls bone growth. The doctor must carefully evaluate and treat this injury in children, so that the finger does not become stunted or deformed.
Nonsurgical Treatment
Most mallet finger injuries are treated with splinting. A splint holds the fingertip straight (in extension) until it heals.
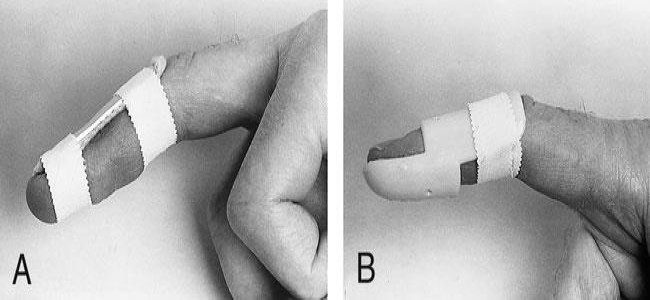
There are several types of splints used to treat mallet finger, many of them fabricated by hand therapists.
To restore function to the finger, the splint must be worn full time for 8 weeks. This means that it must be worn while bathing, then carefully changed after bathing. As the splint dries, you must keep your injured finger straight. If the fingertip droops at all, healing is disrupted, and you will need to wear the splint for a longer period of time.
Because wearing a splint for a long period of time can irritate the skin, your doctor may talk with you about how to carefully check your skin for problems. Your doctor may also schedule additional visits over the course of the 8 weeks to monitor your progress.

When removing the splint for cleaning and drying, the fingertip must stay in extension.
For 3 to 4 weeks after the initial splinting period, you will gradually wear the splint less frequently — perhaps only at night. Splinting treatment usually results in both acceptable function and appearance, however, many patients may not regain full fingertip extension.

A temporary splint is applied with two pieces of tape.
For some patients, the splinting regimen is very difficult. In these cases, the doctor may decide to insert a temporary pin across the fingertip joint to hold it straight for 8 weeks.
Surgical Treatment
Your doctor may consider surgical repair if there is a large fracture fragment, or the joint is out of line (subluxed). In these cases, surgery is done to repair the fracture using pins to hold the pieces of bone together while the injury heals.
It is not common to treat a mallet finger surgically if bone fragments or fractures are not present. Surgical treatment of the damaged tendon usually requires a tendon graft — tendon tissue that is taken (harvested) from another part of your body — or even fusing the joint straight.
An orthopedic hand surgeon should be consulted in making the decision to treat this condition surgically.